The disc is a joint that occupies the ‘space’ that is seen on an X-ray that lies between two vertebrae. 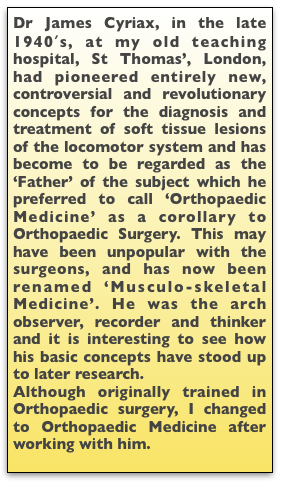
- Sciatica. Mixter and Barr in 1934 described the prolapsed intervertebral disc as a cause of sciatica.
- Backache (LBP). Cyriax JH in the 1940s Suggested that the lumbar flexion on sitting resulted in backward translation of the inter-vertebral disc (IVD) contents was a main element in the cause of backache.
- To this was added the effect of stretching of the ligaments posterior to the lumbar joints.
The anatomy of the Intervertebral Disc.
The intervertebral disc joins two adjacent vertebral bodies allowing the vertebra to move in relation to each other. Individual joint ranges have been given ( excluding the flexion due to pelvic rotation) as are L1 8°, L2 10°, L3 13°, L4 16° & L5/S1 17° (Weingarden DS 1991). It is the sum of ranges at each joint that accounts for the total range of lumbar spinal movement which is very variable depending on age, activities, genetics.
 The intervertebral disc joins two adjacent vertebral bodies allowing the vertebra to move in relation to each other.
The intervertebral disc joins two adjacent vertebral bodies allowing the vertebra to move in relation to each other.
The Nucleus pulposus (NP): Occupies 50-60% of the cross sectional area of the disc, is centrally placed, but lies more posteriorly. It is oval and may have postero-lateral horns and other variations (Jayson MI, 1973). The nucleus is turgid due to osmotic pressure, maintained by high concentrations of proteoglycans and muco-polysaccharides. These are present in a semi-liquid hydrophilic lattice gel system. The intermolecular free water content is approximately 80% ( Hirsh 1952). Being contained in the encircling annulus, it exerts horizontal, hydrostatic pressure and being non-compressible effectively resists and redistributes compression forces (axial loading). It also acts as a shock absorber. It is the largest avascular structure in the body and tends to be starved of metabolic requirements. These have to be supplied by slow diffusion and are helped by the “pumping action” of pressure variations due to changes in posture and respiration.
The Annulus fibrosus (AF) is a ring, anchored to the periphery of the vertebral body above and below and contains the periphery of the pulposus. It consists of 15-25 distinct concentric lamellae of collagen fibrils which are arranged obliquely alternately so that the fibres have an angle of about 50-60˚ to those of the adjacent lamellae. It is especially vulnerable to torsion strains and it may be these that initiate disc degeneration.
Endplates The Superior and Inferior endplates consist of thin discs of cartilage and are part of the adjacent vertebrae, and not strictly a part of the disc. They have to be considered as part of the disc mechanics as they act as junctions between the disc and the adjacent vertebral bodies above and below. Their blood supply allows nutrients to diffuse into the disc. Axial compression results in bulging and fracture at a distortion of 8 mm and is the first structure to fail when the disc is not degenerate.
 Age and degeneration.
Age and degeneration.
Changes due to aging and those due to degeneration are usually considered together but can be distinguished (Adams A, Bogduk Adams, Michael). Aging changes in the disc, both biochemical and biomechanical, start in infancy and are progressive (Kraemer 1995). By the age of 50 disc degeneration is universally present (Andersson 1997). The morbidity curve for discogenic symptoms does not follow the curve for degeneration. The commonest period for symptomatic disc protrusion is the 4th and 5th decades although the process may have started much earlier.
By middle age osmolarity still exists in the nucleus although hydration and proteoglycans are reduced. With degeneration, the stress profile alters with variable and irregular peaks (Adams, Bogduk 2002) and axial loading results in stress peaks particularly in the posterior annulus. This is the area where the disc becomes more vulnerable to breakdown and symptoms are likely to occur.
A degenerate disc is one with structural failure combined with accelerated or advanced signs of aging. This is hastened by
- Damage to the endplates or annulus, which can occur with excessive Intra Discal Pressure (IDP) or strains, particularly if coupled with bending.
- Instability of the motion segment occurs with laxity of the controlling ligaments and atrophy of the deep controlling spinal musculature, the Multifidus muscle complex, which atrophies following joint injury (Hides 1996).
- As ageing (Type II) progresses to degeneration (Type III), the annulus becomes increasingly
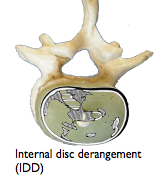 fissured and weakened. A variety of disruptions of the fibres of the annulus are described including radial clefts and peripheral ‘rim’ lesions which are parallel and near the circumference of the disc (Schmorl 1971) and are easily detected, markers of impaired disc function.
fissured and weakened. A variety of disruptions of the fibres of the annulus are described including radial clefts and peripheral ‘rim’ lesions which are parallel and near the circumference of the disc (Schmorl 1971) and are easily detected, markers of impaired disc function.
These, and fissures in the endplates due to excessive compressive forces hastens further nuclear degeneration and are likely to lead to nucleus pulposus prolapse. (Vernon-Roberts 1975).
- Cyriax emphasised that radiological evidence of OA, in the absence of relevant physical signs, was irrelevant to clinical diagnosis (Cyriax JH. 1945).
- Excessive spinal loading augmented by spinal flexion occurs on upright sitting.
- Immobility results in reduced nutrition of the disc.
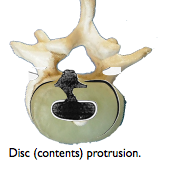 Spinal breakdown may ultimately occur with excessive biomechanical trauma which can be described in engineering terms – compression; torque; sheering; bending moments; distraction. Motion segments where the disc was intact failed, in vitro, at an average torque of 881.4×106 dyne-centimetres (Farfan 1970). Although it has been shown that an intact intervertebral disc can withstand a considerable direct compressive force, this changes in the commonly degenerate disc, when combined with flexion. The nucleus is then liable to protrusion, prolapse and extrusion (Adams et al.,2000b; Natarajan et al., 2004).
Spinal breakdown may ultimately occur with excessive biomechanical trauma which can be described in engineering terms – compression; torque; sheering; bending moments; distraction. Motion segments where the disc was intact failed, in vitro, at an average torque of 881.4×106 dyne-centimetres (Farfan 1970). Although it has been shown that an intact intervertebral disc can withstand a considerable direct compressive force, this changes in the commonly degenerate disc, when combined with flexion. The nucleus is then liable to protrusion, prolapse and extrusion (Adams et al.,2000b; Natarajan et al., 2004).
In old age the lumbar lordotic curve, which in early childhood is secondary to the need to stand upright, eventually reverts back towards the primary prenatal curve into flexion. The disc wedge shape is lost and there is osteoporotic wedging of the vertebral bodies. Disc prolapse in the elderly is rare as the disc tends to be contained by osteophytes and the disc contents are replaced by fibrous tissue resulting in fibrous ankylosis. At this stage the main pathology is due to osteoporosis or spinal stenosis, which is not common.
See Disc Nutrition and movement →
Effect of the upright sitting mode on IVD pathology
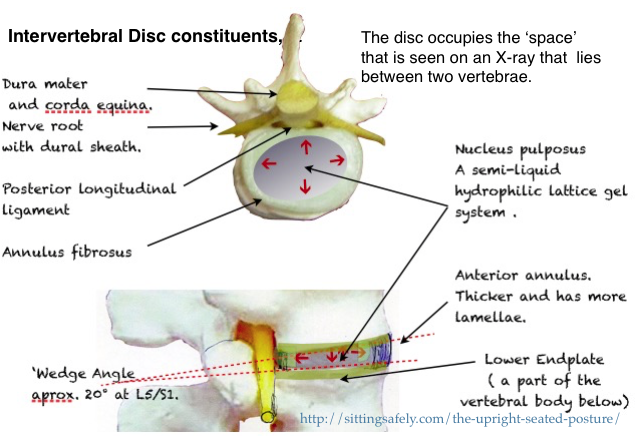
- The conventional mid upright sitting posture causes backward tilting of the pelvis resulting in reduction, or even reversal, of the protective disc wedge angles at the lowest 2 lumbar joints (L4/5 & L5/S1) where mechanical spinal breakdown is commonest.
- Posterior disc protrusion was put forward originally by Cyriax (1945) as the main cause of backache. He also emphasised the importance of the disc wedge angle in preventing prolapse with the adage “Preserve the lumbar lordosis”. For details see ☛ Disc (IVD) angles→
- Gorman showed that This effect is augmented by lumbar support directed to above the L4 vertebra . The predicted effect is retropulsion of the disc contents (NP) and is confirmed by pMRI studies (Smith, 2006).
- •Pelvic tilting also stretches of the lumbo-sacral and supraspinous ligaments which can become irreversible and result in pain and joint instability leading to CTD and earlier degeneration (see Anatomy/Ligaments→).
Clinical effects
If the annulus is unable to contain the increased hydrostatic pressure of the nucleus, while being stressed vertically and simultaneously stretched posteriorly by forward pelvic tilting, retropulsion of the nucleus pulposus becomes more likely. Anterior bulging also occurs and in time becomes contained by osteophytic (‘Parrot’s beaks’ in French) outgrowths from the adjoining vertebral margins. These are evident on x-rays and are silent clinically. This is in contradistinction to disc bulging with a backward or a postero-lateral protrusion where impingement is likely on a number of pain sensitive structures. Herniation or rupture of the annulus can then occur with posterior nuclear or, more commonly, a postero-lateral protrusion which can threaten the emerging nerve root. A large midline extrusion can rupture the posterior longitudinal ligament (PLL) resulting in the surgical emergency of a Corda Equina syndrome
Cyriax and the IV disc. An historical diversion.
Discussion of IV discs and LBP without mentioning Cyriax is equivalent to discussing Natural Selection without mentioning Darwin. Mixter & Barr in the USA having identified IVD prolapse as the main cause of sciatica, Cyriax, at St Thomas’, London, postulated it as the main cause of backache (LBP) (Cyriax JH. 1945). At that time the IVD was regarded as aneural and avascular. I can actually remember a lecture by Prof HA Harris to this effect at Cambridge. so Cyriax had to postulate it’s prolapse and impingement on various adjacent structures as the cause of symptomatology. These included the Posterior Longitudinal Ligament (PLL), the anterior surface of the Dura Mater for ‘extra-segmental’ pain and the dural sheath of the emerging spinal nerves for sciatica, culminating in nerve root conduction loss or, rarely, a cauda equina syndrome. He used a 50 ml. 1/2% Procaine by caudal epidural for confirmation. On various grounds he excluded facet joint, ligaments and the sacro-iliac (SI) joints as causes which degraded his development of a systematic clinical functional examination of the spine but not of peripheral structures. This not only enabled an accurate localisation of soft issue lesions but also diagnosed ‘psycho-genic’ (‘psycho-social’, pg) as a common cause or overlay and that in these cases physical treatment should be avoided. Recently this has come to be considered by some as the main cause of LBP.
 “Lordosis…..directing it (pressure) away from the sensitive structures.” (that lie posterior to the joint, the Ligaments, nerve root, dura mater).
“Lordosis…..directing it (pressure) away from the sensitive structures.” (that lie posterior to the joint, the Ligaments, nerve root, dura mater).
From, Cyriax JH. Illustrated manual of Orthopaedic Medicine. 1982. p. 140
At that time some of Cyriax’s contemporaries criticised his hypothesis as ‘unscientific’ as it was based mainly on observation and not on his own controlled trials. Subsequently his views have become mainstream and used as a basis for treatment by a large body of therapists, medical and physiotherapeutic, worldwide. Later research showed pain receptors (nociceptors) in the posterior part of the annulus (AF) and the surrounding structures and so could be reconsidered as causes of LBP. This simplified the Cyriax hypothesis as direct impingement was no longer a necessity to explain the varied symptoms. Stretching of the posterior ligaments has also come to be recognised as a nociceptive and etiological factor (See Ligaments/Cumulative trauma disorder→). 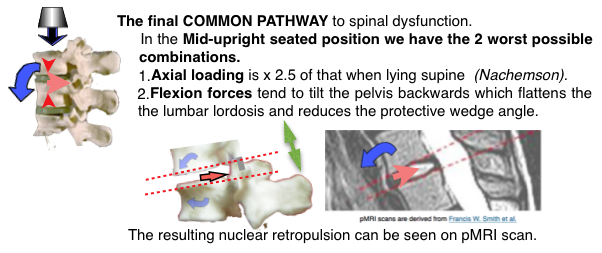
The Cyriax archive devolved to me and I gave it to the ☞Welcome institute for safe-keeping. It included his entire patients notes which are a valuable research resource as they were detailed and systematic.
To continue see detailed sites on the biomechanics factors affecting IVDs. Next see ☛ IV Disc angles→ and the lumbar-sacral junction.
- Or see how this was evolved in ☛ ‘Paleo-anthropology’ ⟶